DOI: 10.1097/SCS.0000000000010073
Abstract
Materials and Methods
Patient Cohort
Image Acquisition and Multimodal Imaging Fusion
All patients’ CT and MRI data (DICOM format) were downloaded from the hospital information system, and then the image data were uploaded to the GE AW workstation. The corresponding image sequences were opened at the workstation, and registration fusion and three-dimensional reconstruction were completed. Automatic registration was first used, and then the fusion function was selected for automatic matching. The Smart Brush function was used to outline the tumor contour, and images such as magnetic resonance angiography and magnetic resonance venography were fused with the tumor to form a three-dimensional digital anatomical image of the tumor and vessels. Finally, the three-dimensional reconstructed image of the skull was added to the display of the tumor’s three-dimensional image with vessels, completing the multimodal imaging fusion.
Surgical Treatment
Results
Clinical Characteristics
Multimodal Imaging Fusion Results
Case Presentation
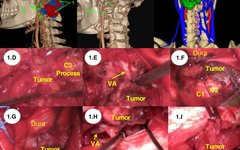
Case 1: A 32-year-old male patient presented with left neck pain for 1 week. Physical examination revealed limited cervical spine movement. MR scan showed a tumor surrounding and compressing the spinal cord. The multimodal fused image was used to design the surgical path and simulate the resection process. An enlarged midline suboccipital approach was adopted to fully expose the anterior and lateral aspects of the tumor. The extradural portion of the tumor was first resected, followed by the subdural portion, ultimately achieving complete tumor resection (Figure 1).
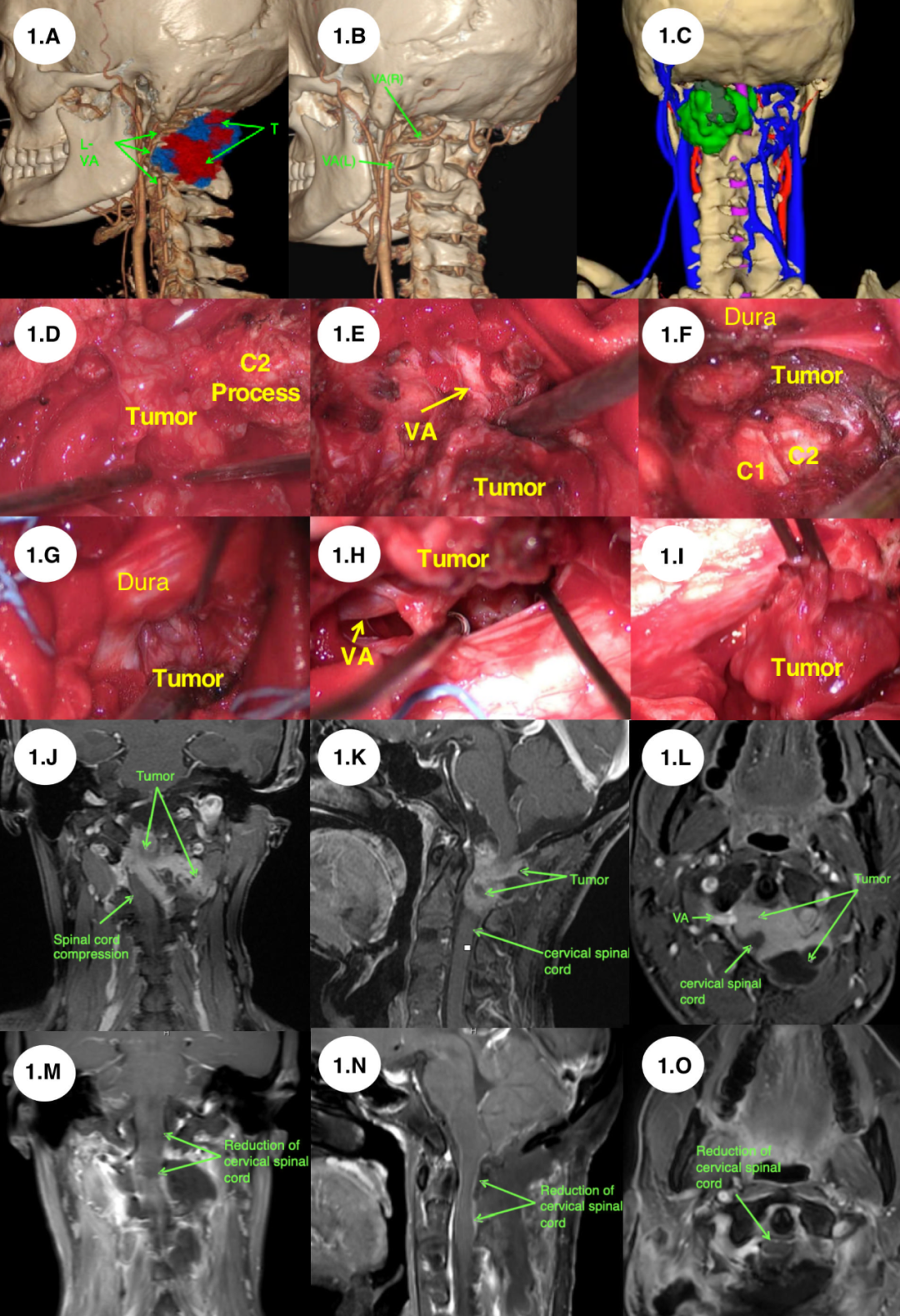
Figure 1. Preoperative multimodal imaging fusion used for approach simulation and surgical treatment of recurrent C2 schwannoma (Case 1). (A-C) Multimodal imaging fusion used to identify the relationship between the tumor, vertebral artery, and bony structures. (D-I) The tumor resection process followed the sequence from extradural to subdural, with the vertebral artery always visible during the tumor resection. (J-O) Comparison of preoperative and postoperative MR scans, achieving complete tumor resection.
Case 2: A 64-year-old male patient presented with left exophthalmos and vision loss for 6 months. Physical examination revealed that the left eyeball was protruding outward due to tumor pressure, with complete loss of vision in the left eye. MR scan showed the tumor with heterogeneous enhancement, widely eroding the anterior skull base. The multimodal imaging fusion was used to design the surgical path and simulate the resection process. An enlarged frontal-temporal approach was adopted, fully exposing the left orbit. The extradural portion of the tumor was first resected, followed by the subdural portion, ultimately achieving complete tumor resection (Figure 2).
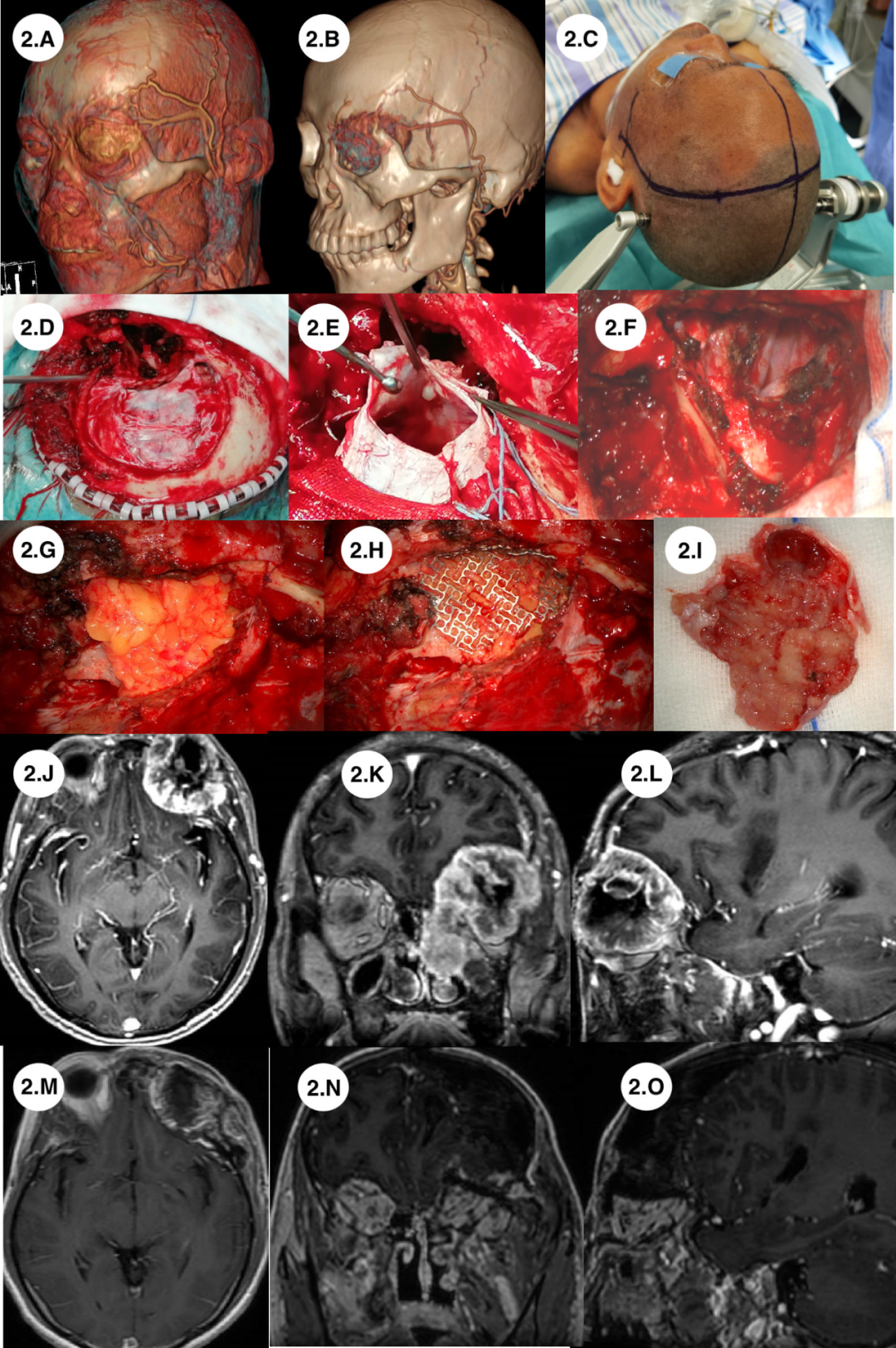
Case 3: A 59-year-old female patient presented with left cheek pain for 2 weeks. Physical examination revealed limited mouth opening. MR scan showed the tumor with heterogeneous enhancement, and CT scan showed erosion of the lateral wall of the maxillary sinus by the tumor. The multimodal imaging fusion was used to design the surgical path and simulate the resection process. The zygomatic arch was removed to fully expose and completely resect the tumor tissue while preserving the coronoid process of the mandible (Figure 3).
Case 4: A 57-year-old female patient presented with right cheek pain for 3 months. Physical examination revealed decreased bite force on the right side. MR scan showed heterogeneous enhancement, and CT scan showed extensive bony destruction in the right infratemporal fossa, with the right temporomandibular joint eroded by the tumor. Computed tomography angiography (CTA) showed that the right internal carotid artery (ICA) and the right external carotid artery were possibly adhered to the tumor. The multimodal imaging fusion was used to design the surgical path and simulate the resection process; however, it clearly showed that the internal carotid artery and external carotid artery were not adhered to the tumor and had almost a 5mm distance. An enlarged middle cranial fossa approach was adopted to fully expose the tumor. First, we opened the extradural tumor, ensuring that the internal carotid artery was not eroded, then made a bone flap to expose the invasive tumor in the right temporal lobe area that entered the subdural space. The tumor was completely resected, and the patient’s temporomandibular joint remained intact, with no neurological functional deficits (Figure 4).
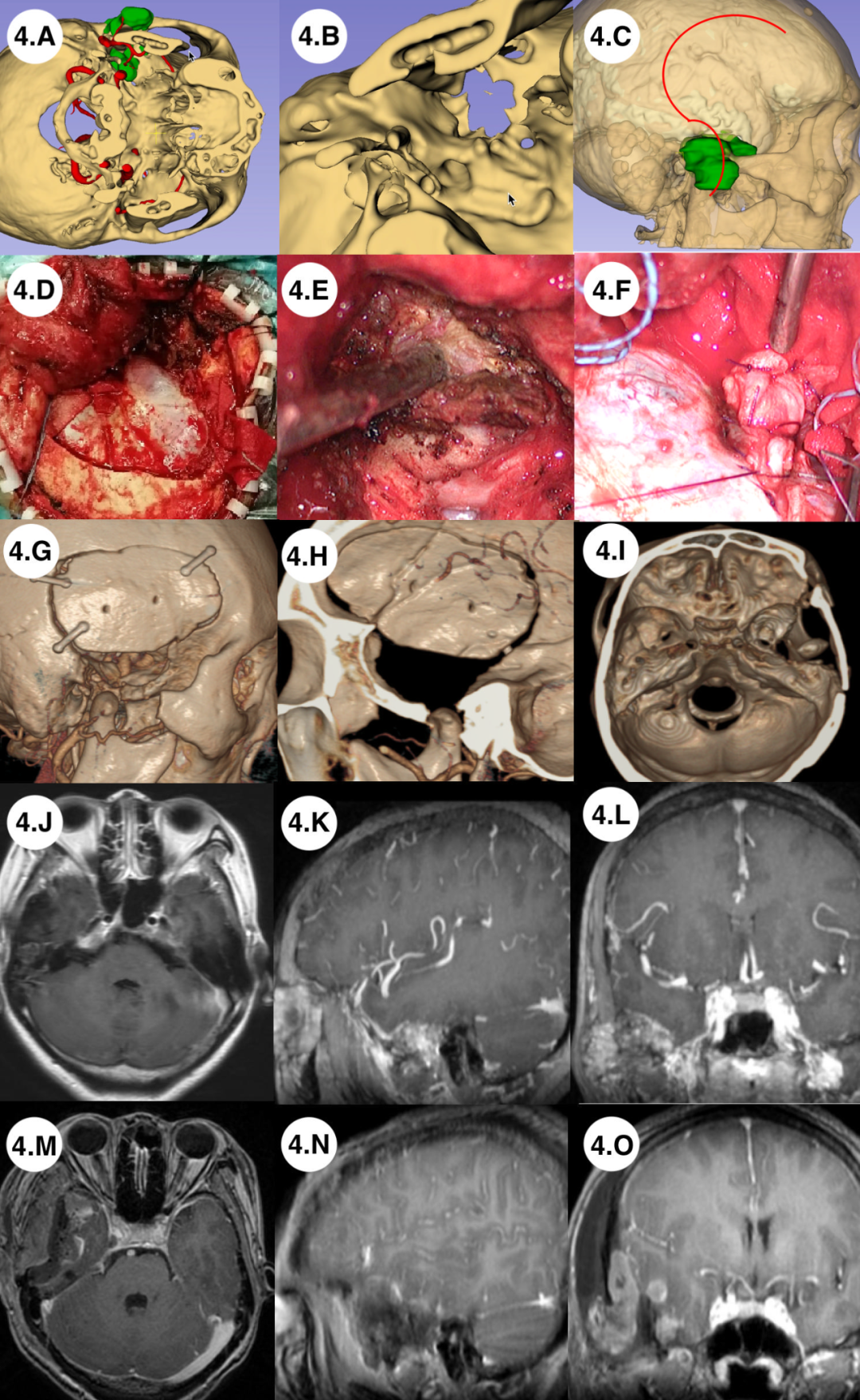
Figure 4. Preoperative multimodal imaging fusion used for approach simulation and surgical treatment of left infratemporal giant cell reparative granuloma (Case 4). (A) Multimodal imaging fusion used to identify the relationship between the tumor and the internal carotid artery, bony defects of the temporal fossa. (B) Showing bony defects of the skull base. (C) Approach and incision designed based on multimodal imaging fusion results. (D) Bone flap lower limit to the temporal base. (E) Tumor resection along the extradural boundary. (F) Reconstruction of the skull base with temporal muscle fascia. (G-I) Postoperative CT reconstruction. (I-O) Comparison of preoperative and postoperative MR scans, achieving complete tumor resection.
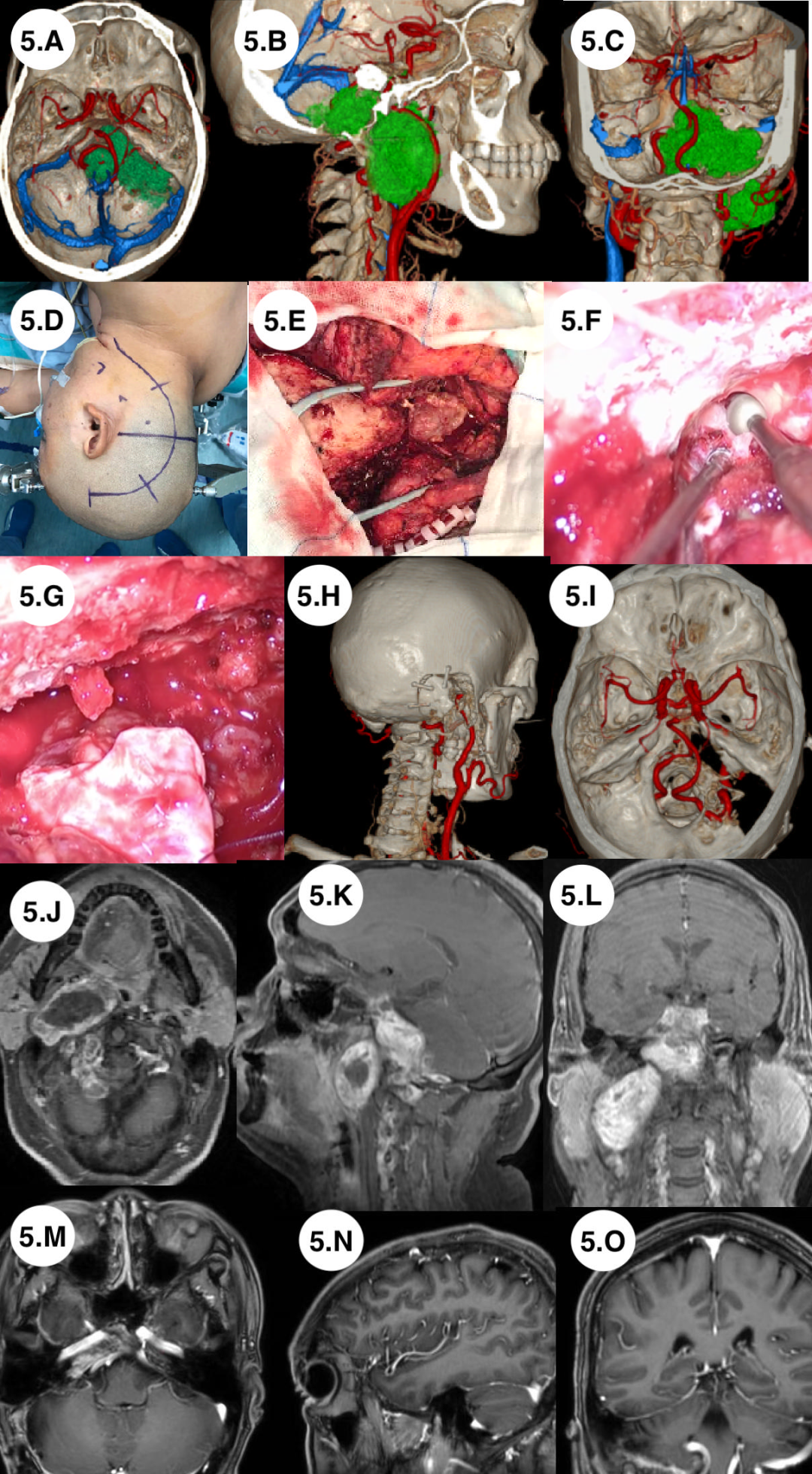
Figure 5. Preoperative multimodal imaging fusion used for approach simulation and surgical treatment of right pharyngeal process lobular malignant tumor (Case 5). (A) Multimodal imaging fusion used to identify the relationship between the tumor and the internal carotid artery, vertebral artery, and the venous sinuses of the middle and posterior cranial fossa. (B) Tumor, internal carotid artery, vertebral artery, infratemporal fossa, and posterior cranial fossa sagittal view. (C) Coronal view of the tumor and arteries. (D) Incision design. (E) Mastoid and tumor exposure; (F) Tumor invading the sigmoid sinus. (G) After sufficient drilling and exposure, resection of the tumor tissue invading the sigmoid sinus. (H-I) Internal carotid artery and vertebral artery preserved intact. (J-L) Preoperative MR scan and postoperative MR scan.
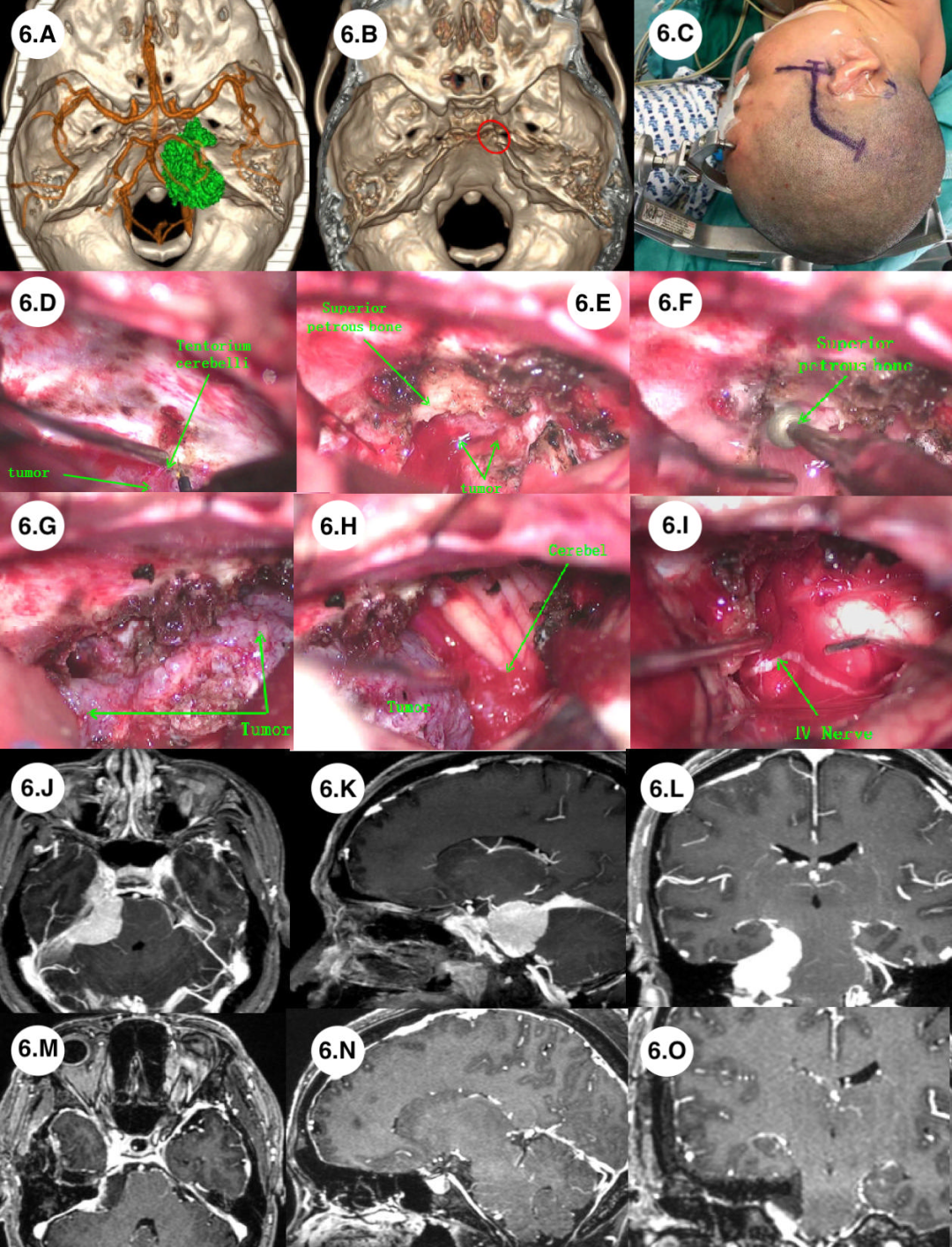
Case 6: A 47-year-old female patient presented with right cheek pain for 4 months. Physical examination revealed right facial numbness. MR scan showed heterogeneous enhancement, and CT scan showed extensive bony destruction in the right infratemporal fossa, with the right temporal apex eroded by the tumor. An enlarged middle cranial fossa approach was adopted to fully expose the tumor. A drill was used to expose the tumor at the petrous ridge, and complete resection was performed, with no neurological functional deficits (Figure 6).
Discussion
Surgical Method Design and Surgical Simulation
Complex skull base tumors are often accompanied by extensive skull base invasion, making single traditional surgical methods unable to completely resect the tumor. Preoperative multimodal imaging fusion and reconstruction may be an important method for formulating individualized surgical approaches. In Case 5, a 39-year-old male was diagnosed with a right parapharyngeal malignant tumor. Preoperative multimodal imaging fusion and three-dimensional image reconstruction clearly showed that the tumor was located in the left parapharyngeal space, invading the cistern, right petrous bone, and right sigmoid sinus. The tumor had a wide range of invasion, and traditional surgical approaches could not simultaneously expose intracranial and extracranial tumors. After preoperative multimodal fusion, a highly lateral approach was designed using 3D images, with an arched scalp incision turning anteriorly, exposing bony structures such as the parapharyngeal space, right mastoid, right occipital bone, and right occipital foramen. Both the right internal carotid artery and the right vertebral artery were clearly exposed during the surgery. Since the right sigmoid sinus was invaded and occluded by the tumor, we resected the right mastoid bone without changing position and directly removed the tumor. The extracranial portion of the tumor was completely resected along the parapharyngeal space, and the intracranial tumor in the CPA region was completely resected. Due to the sufficient exposure of the internal carotid artery, vertebral artery, and other structures, all vessels were well protected. Postoperatively, the patient experienced temporary swallowing difficulties due to interference with the glossopharyngeal nerve during tumor resection. After tracheostomy and rehabilitation treatment, swallowing function recovered after 6 months.
Multimodal imaging fusion and 3D reconstruction can assist neurosurgeons in simulating surgical procedures. Visualizing the surgical position and exposure, as well as the tumor and surrounding structures, is of great significance for surgical planning. In Case 3, for the lobular tumor in the left infratemporal fossa, we simulated the tumor resection process based on multimodal imaging fusion, finding that sufficient surgical space for complete tumor resection was still available while only cutting the zygomatic arch and preserving the coronoid process. It was confirmed that the actual surgical process was consistent with the simulation. After complete tumor resection, the zygomatic arch was preserved.Multimodal imaging fusion technology improves surgical precision and reduces surgical trauma.
Vascular Protection
In terms of vascular protection, based on multimodal 3D reconstruction, the relationship between vessels, tumors, and surrounding structures can be vividly displayed. In Case 1, a 29-year-old patient with recurrent C2 schwannoma, we found that the vertebral artery was located ventrally to the tumor, which helped us determine the safe area for tumor resection. We used a midline suboccipital approach, first identifying the vertebral artery, then separating the tumor along the vertebral artery path. Ultimately, the tumor was completely resected, perfectly preserving the vertebral artery. Additionally, in Cases 4 and 6 with petrous region tumors, multimodal imaging fusion vividly displayed the relationship between the internal carotid artery and the tumor, and this preoperative information helped us confidently protect the arteries during the surgery.
Skull Base Reconstruction
Preoperative multimodal imaging fusion and reconstruction technology can display the tumor and surrounding structures in three dimensions. Compared to traditional 2D images, it can provide comprehensive image information for surgeons preoperatively, including the extent of the tumor and the area of skull bone invasion. In Case 2, a 52-year-old male was diagnosed with a right orbital-anterior skull base recurrent spindle cell tumor, which grew into the intracranial and extracranial regions through the ethmoid sinus and superior orbital fissure. Preoperative three-dimensional images clearly showed multiple directions of bony defects in the lateral wall of the orbit, the sella turcica, and the medial wall of the orbit. We adopted a frontal-temporal approach during the surgery. Preoperatively, appropriately sized titanium plates were prepared based on the area of bony defects. During the surgery, the frontal bone surface was preserved, and the titanium plate reconstructed the orbital wall and anterior skull base structures, with no cerebrospinal fluid leakage occurring postoperatively. Image fusion provided a spatial anatomical relationship of the skull defect and a visual display of quantitative data, which is beneficial for tumor resection and skull base reconstruction.
Complications
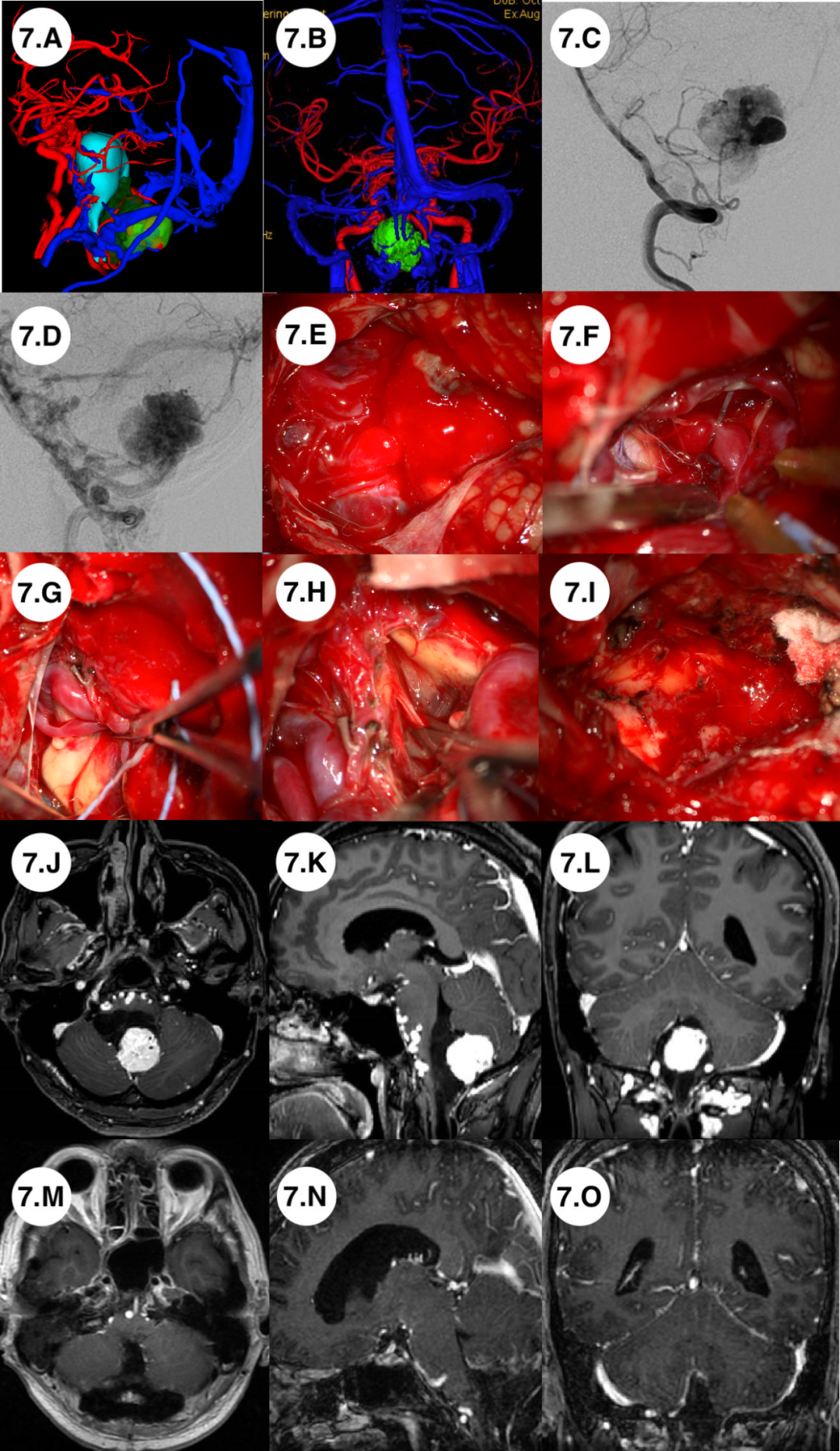
Cerebrospinal fluid leakage is the most common complication of complex skull base tumor surgery. The basic principle we follow is to be careful and gentle when separating the tumor attached to the meninges during the surgery to maintain the integrity of the tumor. When resecting the tumor during the surgery, care should be taken to preserve the residual meninges of the skull base and not to excessively resect the meninges in emphasizing complete tumor resection. In these cases, none of the patients experienced cerebrospinal fluid leakage. Protection of cranial nerves should also follow the same principle. One case of parapharyngeal interstitial malignant tumor resulted in postoperative swallowing difficulties due to the high adhesion between the glossopharyngeal nerve and the tumor. In Case 7, a fourth ventricle vascular embryonal tumor accompanied by vascular malformation resulted in brainstem infarction due to preoperative vascular embolization, leading to coordination issues in the patient. During the surgery, all vessels were well protected, and the coordination issues resolved after 3 months of conservative treatment.
Practicality and Limitations of 3D Multimodal Software
Regarding the software for preoperative multimodal imaging fusion technology, this study mainly used the GE-AW workstation, which has significant advantages in multimodal imaging fusion of the brainstem, cranial nerves, vessels, and skull. However, it also has some disadvantages, including that the details of skull reconstruction are not as precise as in 3D slicer, which can display various structures of the skull in higher resolution. To achieve better performance in reconstruction, the MR and CT scan thickness should be 2.0mm or less.
Conclusion
The choice of surgical approach depends on the growth characteristics of the tumor and the extent of venous or sinus involvement. Preoperative multimodal imaging fusion technology can provide a wealth of valuable visual information for skull base tumor surgery. For complex skull base tumors, due to their deep location and complex anatomical relationships, preoperative surgical simulation based on multimodal imaging fusion can ensure a safer surgical process.
Swipe up to read
1. Singh AK, Srivastava AK, Sardhara J, et al. Skull base bony lesions: Management nuances; a retrospective analysis from a Tertiary Care Centre. Asian J Neurosurg. 2017;12(3):506-513. doi:10.4103/1793-5482.185068
2. Khanapure K, Joshi KC, Jagannatha AT, et al. Supraorbital Craniotomy for Large Anterior Skull Base Meningiomas: A Technical Note. Asian J Neurosurg. 2019;14(3):767-772. doi:10.4103/ajns.AJNS_40_19
3. Kalra GS, Midya M, Bedi M. Access to the Skull Base – Maxillary Swing Procedure – Long Term Analysis. Ann Maxillofac Surg. 2018;8(1):86-90. doi:10.4103/ams.ams_5_18
4. Liu JK, Zhao K, Baredes S, Jyung RW. Extended Anterolateral Infralabyrinthine Transjugular Approach for Microsurgical Resection of Giant Glomus Vagale Tumor: Operative Video and Technical Nuances. J Neurol Surg B Skull Base. 2021;82(Suppl 1):S59-S60. doi:10.1055/s-0040-1716532
5. Malekpour M, Cohen-Gadol AA. The pursuit of a cholesteatoma by harvey cushing: staged approach to a complex skull base tumor. J Neurol Surg B Skull Base. 2014;75(5):339-345. doi:10.1055/s-0034-1372471
6. Liu H, Qian H, Li X, et al. Clinial Features, Individualized Treatment and Long-Term Surgical Outcomes of Skull Base Meningiomas With Extracranial Extensions. Front Oncol. 2020;10:1054. Published 2020 Jun 30. doi:10.3389/fonc.2020.01054
7. Ito S, Saegusa T, Ozawa Y, et al. Function-Preserving Multimodal Treatment for Jugular Foramen Meningiomas. J Neurol Surg B Skull Base. 2019;80(3):239-243. doi:10.1055/s-0038-1668137
8. Bonne NX, Dubrulle F, Risoud M, Vincent C. How to perform 3D reconstruction of skull base tumours. Eur Ann Otorhinolaryngol Head Neck Dis. 2017;134(2):117-120. doi:10.1016/j.anorl.2016.09.003
9. Thust SC, Yousry T. Imaging of skull base tumours. Rep Pract Oncol Radiother. 2016;21(4):304-318. doi:10.1016/j.rpor.2015.12.008
10. Oishi M, Fukuda M, Ishida G, Saito A, Hiraishi T, Fujii Y. Prediction of the microsurgical window for skull-base tumors by advanced three-dimensional multi-fusion volumetric imaging. Neurol Med Chir (Tokyo). 2011;51(3):201-207. doi:10.2176/nmc.51.201
11. Jian ZH, Li JY, Wu KH, et al. Surgical Effects of Resecting Skull Base Tumors Using Pre-operative Multimodal Image Fusion Technology: A Retrospective Study. Front Neurol. 2022;13:895638. Published 2022 May 12. doi:10.3389/fneur.2022.895638
12. Aghdasi N, Whipple M, Humphreys IM, Moe KS, Hannaford B, Bly RA. Automated Surgical Approach Planning for Complex Skull Base Targets: Development and Validation of a Cost Function and Semantic At-las. Surg Innov. 2018;25(5):476-484. doi:10.1177/1553350618782287
13. Stefko ST. Combined Surgical Approaches In and Around the Orbit. J Neurol Surg B Skull Base. 2020;81(4):472-479. doi:10.1055/s-0040-1713938
14. Ocak PE, Yilmazlar S. Resection of a Lower Clival Meningioma via Posterolateral Approach: Two-Dimensional Operative Video. J Neurol Surg B Skull Base. 2021;82(Suppl 1):S31-S32. doi:10.1055/s-0040-1714407
15. King AD. MR Imaging of Nasopharyngeal Carcinoma. Magn Reson Imaging Clin N Am. 2022;30(1):19-33. doi:10.1016/j.mric.2021.06.015
16. Duek I, Sviri GE, Billan S, Gil Z. Minimally Invasive Surgery for Resection of Parapharyngeal Space Tumors. J Neurol Surg B Skull Base. 2018;79(3):250-256. doi:10.1055/s-0037-1607315
17. Touska P, Connor SEJ. Recent advances in MRI of the head and neck, skull base and cranial nerves: new and evolving sequences, analyses and clinical applications. Br J Radiol. 2019;92(1104):20190513. doi:10.1259/bjr.20190513
18. Grosch AS, Schröder T, Schröder T, Onken J, Picht T. Development and initial evaluation of a novel simulation model for comprehensive brain tumor surgery training. Acta Neurochir (Wien). 2020;162(8):1957-1965. doi:10.1007/s00701-020-04359-w
19. Echalier EL, Subramanian PS. Meningiomas of the Planum Sphenoidale and Tuberculum Sella. J Neurol Surg B Skull Base. 2021;82(1):72-80. doi:10.1055/s-0040-1722703
20. Crea A, Grimod G, Scalia G, et al. Fronto-orbito-ethmoidal intradiploic meningiomas: A case study with systematic review. Surg Neurol Int. 2021;12:485. Published 2021 Sep 30. doi:10.25259/SNI_386_2021
21. Antonelli V, Maimone G, D’Andrea M, Tomassini A, Bassi M, Tosatto L. “Single-step” resection and cranio-orbital reconstruction for spheno-orbital metastasis with custom made implant. A case report and review of the literature. Int J Surg Case Rep. 2021;81:105755. doi:10.1016/j.ijscr.2021.105755
22. Thurnher D, Novak CB, Neligan PC, Gullane PJ. Reconstruction of lateral skull base defects after tumor ablation. Skull Base. 2007;17(1):79-88. doi:10.1055/s-2006-959338
23. Swendseid BP, Roden DF, Vimawala S, et al. Virtual Surgical Planning in Subscapular System Free Flap Reconstruction of Midface Defects. Oral Oncol. 2020;101:104508. doi:10.1016/j.oraloncology.2019.104508
24. Totten DJ, Manzoor NF, Yancey KL, Yawn RJ, Haynes DS, Rivas A. Comparison of Small Intestinal Submucosal Graft and Autologous Tissue in Prevention of CSF leak after Posterior Fossa Craniotomy. J Neurol Surg B Skull Base. 2021;82(6):695-699. Published 2021 Mar 12. doi:10.1055/s-0040-1713772
25. Jimbo H, Kamata S, Miura K, Asamoto S, Tada S, Endo T, Masubuchi T, Nakamura N, Fushimi C. Operative management of skull base malignant tumors arising from the nasal cavity and paranasal sinus: recent strategies used in 25 cases. Neurol Med Chir (Tokyo). 2010 Jan;50(1):20-6; discussion 26. doi: 10.2176/nmc.50.20. PMID: 20098020.
26. Adeleye AO. A giant, complex fronto-ethmoidal ivory osteoma: Surgical technique in a resource-limited practice. Surg Neurol Int. 2010;1:97. Published 2010 Dec 31. doi:10.4103/2152-7806.74489
27. Klironomos G, Chiluwal A, Dehdashti AR. Staged Approach for Petroclival Meningioma Resection. J Neurol Surg B Skull Base. 2019;80(Suppl 3):S308-S309. doi:10.1055/s-0039-1677849
28. Abu-Ghanem S, Fliss DM. Surgical approaches to resection of anterior skull base and paranasal sinuses tumors. Balkan Med J. 2013;30(2):136-141. doi:10.5152/balkanmedj.2013.9112
29. Hu S, Arnaoutakis D, Kadakia S, Vest A, Sawhney R, Ducic Y. Osseointegrated Implants and Prosthetic Reconstruction Following Skull Base Surgery. Semin Plast Surg.2017;31(4):214-221.doi:10.10

Corresponding Author Introduction

Chen Gang, Chief Physician
Zhuhai People’s Hospital
-
Chief physician, Doctor of Medicine, Director of the Department of Neurosurgery, Zhuhai People’s Hospital
-
Standing member of the Neurosurgery Anatomy Branch of the Chinese Anatomical Society
-
Standing member of the Cerebral Hemorrhage Minimally Invasive Treatment Professional Committee of the Chinese Stroke Society
-
Standing member of the Neurosurgical Trauma Branch of the Chinese Association for Medical and Health International Exchange
-
Vice Chairman of the Neurosurgery Professional Committee of the Guangdong Medical Education Association
-
Vice Chairman of the Neurosurgery Professional Committee of the Guangdong Hospital Association
-
Vice Chairman of the Neurosurgery Management Branch of the Guangdong Medical Industry Association
-
Chairman of the Neurosurgery Branch of the Zhuhai Physician Association

Scan the QR code to visitChen Gang, Chief Physician‘s academic homepage
See more wonderful content
First Author Introduction

Jian Zhiheng, Associate Chief Physician
Zhuhai People’s Hospital
-
Associate Chief Physician, Master’s Degree from Southern Medical University, Master’s Supervisor at Guangdong Medical University
-
Executive member of the Neurosurgery Information Application Branch of the Guangdong Health Information Network Association
-
Youth member of the Neurosurgical Oncology Branch of the Guangdong Medical Association
-
Member of the Neurosurgery Branch of the Guangdong Medical Education Association
-
Executive member and secretary of the Neurosurgery Branch of the Zhuhai Physician Association
-
Member of the Neurosurgery Branch of the Zhuhai Medical Association
-
In the past 3 years, hosted one municipal-level project, published 4 SCI papers as the first author, and 1 CSCD paper.

Click “Read Original Text” to view the original text.