MCP and PIP Joint Arthroplasty

The function of the metacarpophalangeal (MCP) joint and proximal interphalangeal (PIP) joint in the hand is crucial for daily activities (ADLs), and the likelihood of degenerative changes is significant. Joint arthroplasty of the small joints of the hand, particularly MCP and PIP joints, is a widely accepted method for treating symptomatic arthritis. Arthroplasty of small joints has shown significant efficacy in treating joint pain, restoring joint range of motion, and improving overall hand function. Both silicone and surface-replacement prostheses (graphite or metal) can be used for MCP and PIP joints.

MCP Joint Arthroplasty
The surgical technique for arthroplasty using silicone and surface replacement is similar, typically accessed via a dorsal approach to the MCP joint. A longitudinal central incision is made on the dorsal side of the affected single MCP joint. If multiple MCP joints are targeted at once, a transverse incision can be made along the center of the joint. Care must be taken to protect the sensory nerve branches. In patients with rheumatoid arthritis, the extensor tendons often subluxate ulnarly, so the extensor tendon cap is cut on the ulnar side of the extensor tendon. If the tendon is not subluxated, a longitudinal incision can be made, and it can be repaired during closure. Next, the joint capsule is opened, and synovectomy is performed to remove the extensively proliferated synovial tissue. The distal part of the metacarpal is excised from the distal end of the collateral ligament. When using silicone grafts, simply place the distal part of the silicone graft into the bone tunnel of the proximal phalanx without removing the subchondral bone. For surface implants, osteotomy of the metacarpal and phalanx is performed with the help of fluoroscopy, using calibrated cones. While using the calibrated cone, continuously increase the drill bit size to open the medullary cavity. Use experimental models to test the size of the prosthesis for appropriateness and joint stability and range of motion while using fluoroscopy to determine the position of the prosthesis and repair the dorsal joint capsule and extensor tendon. Postoperatively, the hand is placed in a larger padded palm splint, with the MCP joint flexed and the PIP joint extended. If the joint feels relatively loose postoperatively, the size of the prosthesis needs to be reassessed, or the postoperative rehabilitation may need to be more conservative.
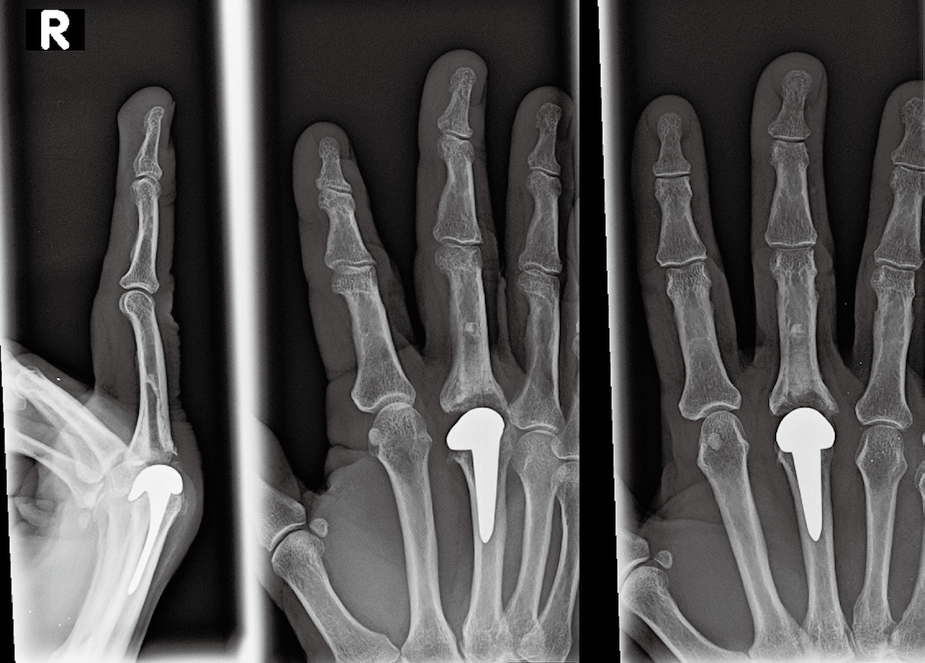
Posteroanterior, lateral, and oblique X-ray images following high-temperature graphite material arthroplasty of the middle finger MCP joint.
Posteroanterior X-ray images following silicone material arthroplasty of the index, middle, ring, and little fingers MCP joints.
PIP Joint Arthroplasty
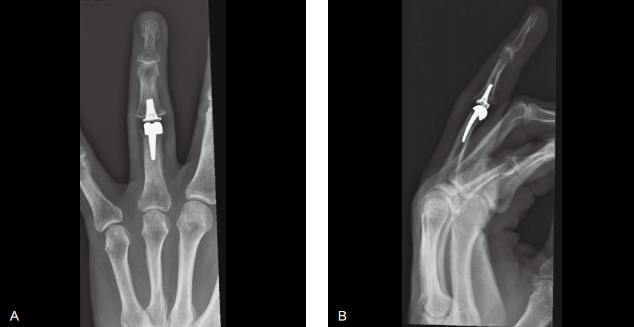
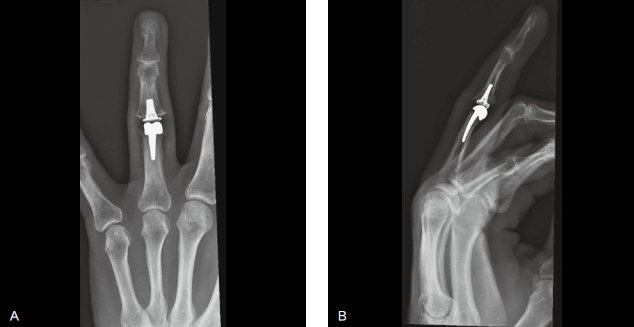
A. Posteroanterior X-ray images after PIP joint arthroplasty; B. Lateral X-ray images after PIP joint arthroplasty.
Postoperative Rehabilitation
Postoperative Interventions
● Wound Care: After the large gauze is removed, use a light pressure bandage. Dressing changes need to be done at a rehabilitation center or physician’s care center until the wound is fully healed. 2 weeks or so, start scar massage after the stitches are removed until the wound fully heals.
● Swelling Management: Light elastic bandages, such as self-adhesive bandages, can be used on the fingers and palms to maintain active ROM training of the shoulder, elbow, wrist, and fingers during the first few weeks after surgery, which can reduce upper limb swelling. Patients should continuously keep their hands elevated while seated during the first few weeks.
● Orthotics: 2 different combinations of orthotics, one for daytime use and another for nighttime use.
● Daytime orthotics are used to maintain ROM.
 .
.
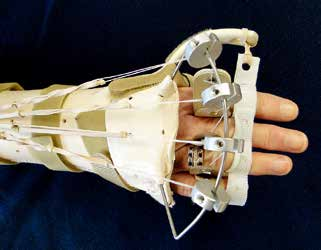
Dynamic orthotics used within 6-8 weeks after MCP joint arthroplasty, equipped with lightweight suspension rings, with the MCP joint in an extended position.

This orthotic allows flexion activity of the MCP joint.
● Combined into a dynamic extension orthotic for the forearm dorsal hand.
● Through external splints and finger suspension rings around the fixed proximal phalanx, passive extension of the MCP joint is achieved through the tension of elastic bands.
● The orthotic fixes the wrist in a neutral position, with the MCP joint at 0° or slight flexion, allowing the MCP joint to actively flex up to 70°, and can return to the resting position under the power of the elastic band, ensuring normal alignment of the fingers.
● It is essential to adjust the tension of the dynamic extension orthotic to avoid excessive extension of the MCP joint, paying attention to the position of the 5th MCP joint, as it is prone to overextension.
● Use X-ray or fluoroscopy to determine if the MCP joint is in a state of excessive extension within the orthotic. Patients can demonstrate or report that the force generated by flexing and extending the MCP joint can easily counteract the tension of the elastic band. Under this lightweight suspension ring, actively flexing the fingers requires about 40% more force, and most patients tend to prefer this lightweight suspension ring. The size of the force needs to be adjusted very carefully.
● For patients with repair of the radial collateral ligament of the index finger, an additional supination protection device should be worn during training.
The supination device of the orthotic is used to protect the radial collateral ligament.
● Nighttime orthotics for fixation: Because the external splint orthotic is inconvenient to use at night, a palmar orthotic is used to fix the wrist and fingers in a neutral aligned position.
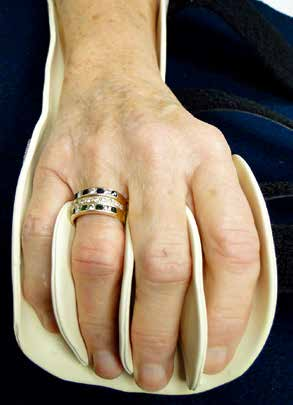
The nighttime splint has a guiding groove for the hand to ensure its normal position.

The protective strap enhances the alignment of the fingers in a neutral position.
● The corrective splint is elevated on the ulnar side to prevent movement toward the ulnar side. The protective strap and interdigitating splint are connected to the splint, forming a guiding groove to ensure the fingers are aligned in a neutral position.
● Nighttime orthotics are typically used for several months postoperatively to maintain the collateral ligaments in a natural, relaxed position, and to assist in restoring joint alignment through long-term ligament balance.
● Rehabilitation Training: Focus on MCP joint activity.
● 1-4 weeks
● During the first rehabilitation treatment period, conduct active and gentle passive ROM training.
● All ROM training will affect scar formation at the wound; active ROM can help control postoperative swelling. Practice once every hour.
● Measure ROM before and after each treatment to monitor finger extension lag. If there is a lag in finger extension (> 30°), passive flexion training needs to be stopped.
● 2-3 weeks: The MCP joint flexion should reach at least 50°. If not achieved, additional orthotic intervention is needed.
○ Need to use a PIP joint sleeve to prevent PIP joint activity, focusing on MCP joint activity.

The proximal interphalangeal joint sleeve prevents movement of the proximal and distal interphalangeal joints, while allowing movement of the MCP joint.

The sleeve allows movement of the MCP joint.
○ Assisted with static progressive or dynamic MCP joint flexion movement.
● 3 weeks: The joint capsule heals, providing sufficient joint stability, and the patient can perform AROM training without the help of dynamic orthotics.
● 4-6 weeks: Simple ADLs can be performed without using orthotics.
● Safe activities include not very tight or forceful gripping or pinching actions, and avoiding actions that require ulnar pressure on the fingers in ADLs.
● Patients should be informed and taught the essentials of joint protection, including how to adjust their movement patterns, how to grip, how to manage pain, and increase grip strength.
● If there is ulnar deviation observed during activities, a hand orthotic should be worn to ensure active ROM and proper alignment of the fingers.
● If the extension lag angle of the extensor muscles is > 30°, the patient needs to continue wearing the dynamic extension orthotic.
● 6-8 weeks
● Continue the rehabilitation training content from 0-6 weeks.
● Continue ROM training and control edema.
● The daytime dynamic orthotic may no longer be used.
● However, nighttime orthotics still need to be used.
● 8-12 weeks
● If needed, light functional strength training can begin. Ensure good finger alignment during training to avoid abnormal stress.
● If active extension function is satisfactory, but flexion range is not, continue using the dynamic flexion orthotic.
● Home Program
● Nighttime orthotics need to continue being used until 6 months post-surgery. No long-term activity restrictions or precautions.
This treatment plan aims to provide general guidance. It is worth noting that there is currently no consensus on when rehabilitation treatment must begin, when to use orthotics, or whether alternating between static flexion and static extension orthotics is effective. Similarly, there are no specific detailed requirements regarding when daytime or nighttime orthotics should not be used. Rehabilitation after MCP joint arthroplasty requires professional rehabilitation therapists to combine each patient’s tissue response to surgery and treatment interventions with clinical reasoning to determine a personalized treatment plan.
PIP Joint Arthroplasty
Postoperative Interventions
● Wound Care: After the large hemostatic gauze is removed, a lightweight elastic bandage can be used to wrap the wound; dressing changes should be done in a professional therapist’s or physician’s clinic. After the stitches are removed, scar massage should be performed until the wound fully heals, approximately 2 weeks later.
● Swelling Management: Light elastic bandages, such as self-adhesive bandages, can be used on the fingers and hand; maintaining normal AROM of the shoulder, elbow, wrist, and finger joints during the first few weeks after surgery can reduce upper limb swelling. Patients need to keep their hands elevated while seated during the first few weeks.
● Orthotics
● 1-5 weeks
● Use static hand splints.
● The MCP joint is in a 15° flexed position.● The PIP joint is maintained in a 15°~30° flexed position to increase joint stability and prevent hyperextension.
● A recent study indicates that the results obtained using static orthotics are similar to those with dynamic orthotics. Static orthotics are less costly and easier for clinical practitioners to manage and apply.
● Patients need to use X-ray fluoroscopy to ensure that the PIP joint is not in a state of hyperextension while wearing the splint.
● 6-11 weeks
● Continue using nighttime orthotics for about 2 weeks, allowing the joint to rest after using the hand for ADLs.
● No longer need to use orthotics. Patients begin using their hands to perform simple activities and exercises without the use of extension-limiting sleeves. By around 6 weeks post-surgery, the joint tissue is sufficiently scarred in a slightly flexed position.
● Rehabilitation Exercises
● AROM training for the MCP and DIP joints as shown in the images.3-4 weeks of extension tendon repair requires fixation of the PIP joint to facilitate movement of the MCP and DIP joints while reducing sliding of the extensor tendon in that area.


Ring static orthotics can prevent movement of the proximal interphalangeal joint while allowing movement of the metacarpophalangeal and distal interphalangeal joints.
● PIP joint short arc motion (short arc motion,SAM): AROM training within the orthotic of –15°~35°; the MCP joint remains in an extended position, with the wrist in a slight flexed position. Early AROM training can reduce swelling and tendon adhesions. Limit hyperextension to prevent the prosthesis from being in a hyperextended position. In the absence of lagging of the extensor, active flexion can enhance by 10° per week.


The short arc motion orthotic allows active flexion of the proximal interphalangeal joint to 35° and extension to –15°.
● 6-11 weeks
● Orthotics
● Rehabilitation Exercises
● Appropriate ADLs can help regain functional strength, avoiding the risk of excessive stress leading to swelling and pain.
● If the collateral ligament is damaged during surgery, resistance training should be avoided at 6 weeks, as this may lead to joint instability. Resistance training may also cause pain.
● 12 weeks: Until the patient achieves normal functional strength.
● Rehabilitation Exercises: Begin light resistance training (light grip exercises or assisted hand training) to help regain functional strength.