This article is authorized to be reproduced by WeChat public account “Chatting Immunology”.
Mast Cells (MC) Development Classification and Functions

Mast cells evolved in sea squirts 500 million years ago, providing the host with natural immunity against bacteria and parasites. Over thousands of years, MC has acquired additional functions regulating inflammation, wound healing, coagulation, adaptive immunity, and acute allergic reactions.
Hematopoietic stem cells (HSC) differentiate into mast cells through multiple stages.
Mast Cell Development
Bone Marrow Differentiation Stage (Multipotent Progenitor [MPP], Common Myeloid Progenitor [CMP], Granulocyte/Macrophage Progenitor [GMP], Basophil/Mast Cell Progenitor [BMCP]), then producing Mast Cell Progenitors (MCP). MCP spreads intothe bloodstream, and then entersthe tissues, where they further differentiate into mature non-proliferative granule-positive mast cells (MC).
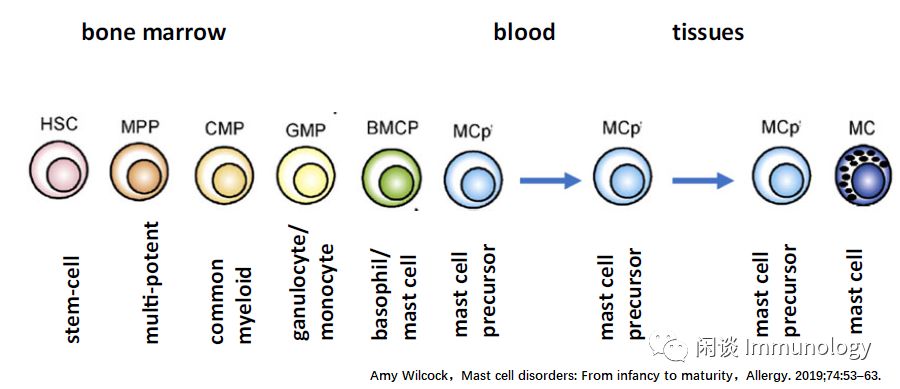
MCs are non-proliferative long-lived resident immune tissue cells, different from Common Myeloid Progenitors (CMPS).
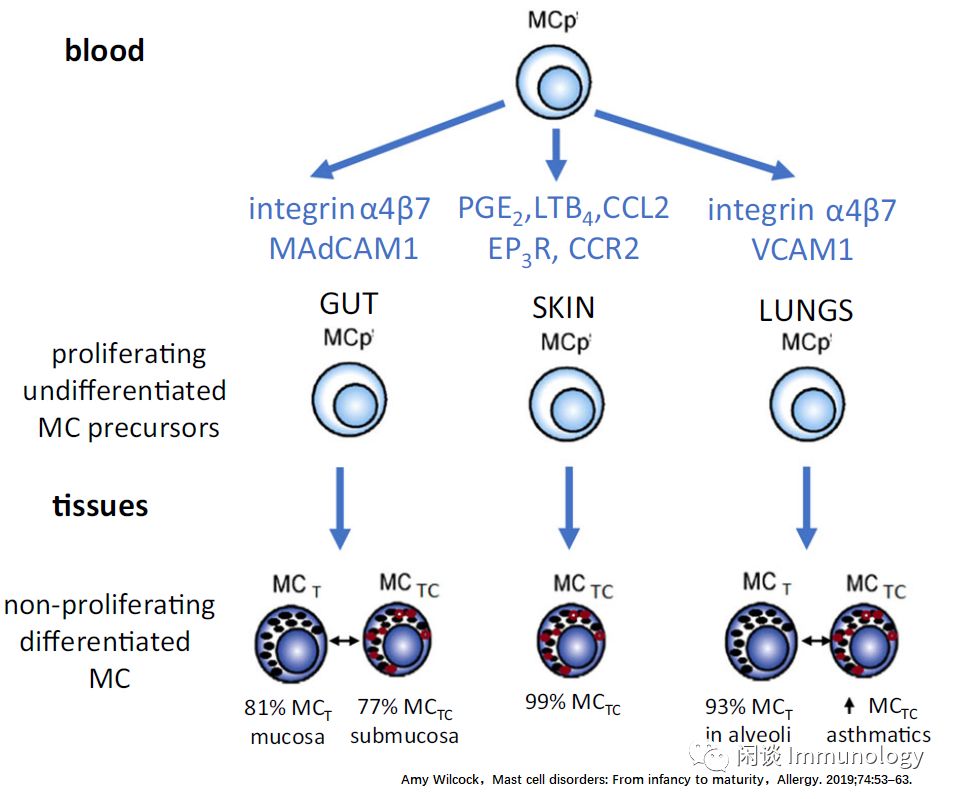
Immature MC precursors (MCP) have proliferative potential, leaving the bone marrow and homing to epithelial tissues such as skin, respiratory tract, and intestine mediated by integrins and chemokine receptors.
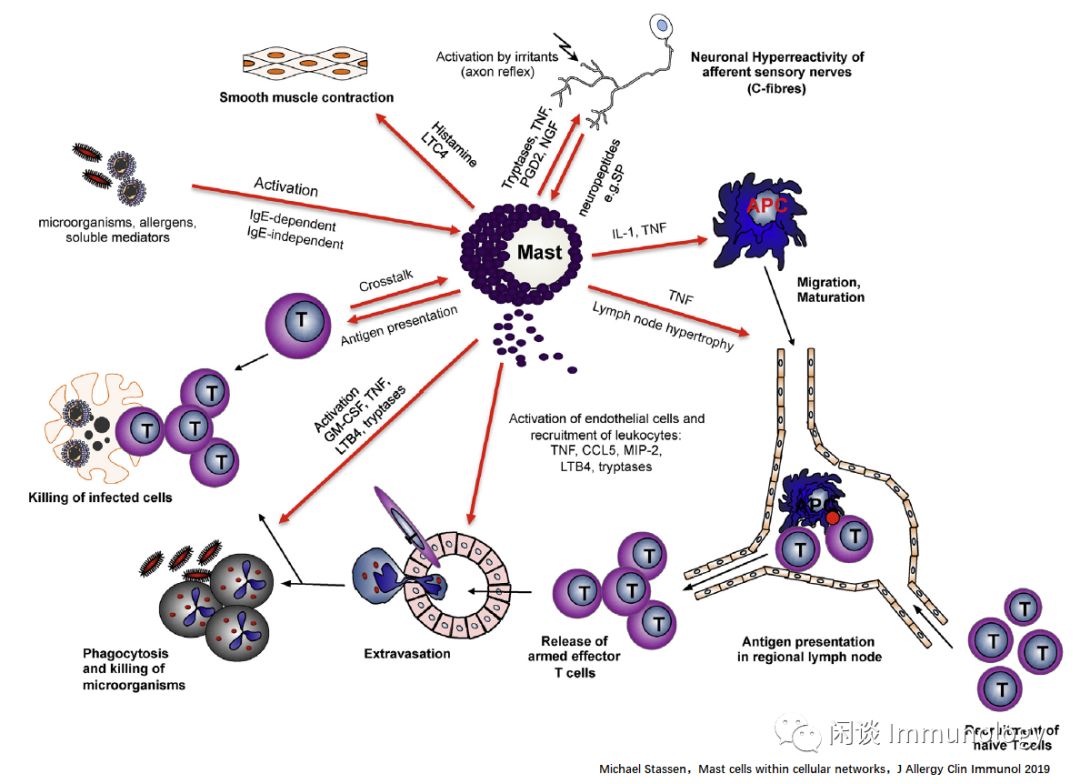
Upon activation, MCs release inflammatory mediators (histamine, tryptase, carboxypeptidase, and other serine proteases) through phospholipid membrane metabolism (platelet-activating factor, leukotrienes, prostaglandins), cytokines (TNF-α, IL-4), and chemokines (IL-8, Monocyte Chemoattractant Protein 1 [MCP-1]).
Mast Cell Classification and Functions
Mature human MCs are typically divided into two subpopulations.MCTC expresses tryptase, chymase, carboxypeptidase, and tissue peptidase, dominating in connective tissues and skin.
MCT expresses tryptase but no other serine proteases, dominating in healthy lung parenchyma and intestinal mucosa. Inflammatory cytokines like IL-4 can alter the balance between MCT and MCTC in the lungs, leading to a dominance of MCTC in asthma patients. The interconversion between MC subtypes depends on the microenvironment.
The two MC subpopulations have different functional and clinical significances; MCT is activated through cross-linking of surface Fc (RI leading to classic IgE-mediated hypersensitivity reactions). In contrast, MCTC expresses high levels of Mas-related G protein-coupled receptor X2 (MRGPRX 2), which activates cytoplasmic calcium release via the phospholipase C pathway.
MRGPRX2 can be activated by endogenous peptides such as substance P, allergen C3a, C5a, VIP, and drugs like morphine, vancomycin, sulfa drugs, and cisatracurium.
Activation of MRGPRX2 on MCTC induces a rapid but less granule release-like allergic reaction. MRGPRX2 activation is also important in chronic spontaneous urticaria. The released gastrin-releasing enzyme directly from MCTC converts angiotensin I to angiotensin II, possibly contributing to remodeling in vascular asthma, atherosclerosis, and aortic aneurysms.
Mast Cells Regulating Immunity

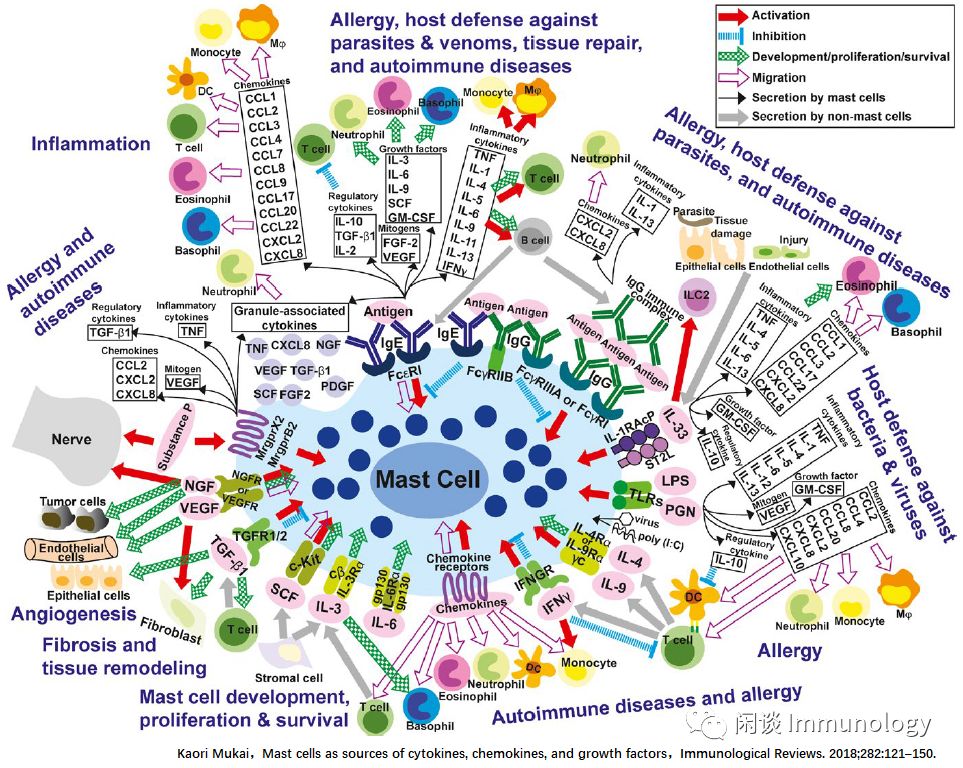
Mast Cells (MC) mainly release three types of factors: Activation, Inhibition, and Migration.
In adaptive immune responses (such as those triggered by parasites, animal venoms, or allergens), IgE cross-links with bivalent or multivalent antigens and binds to the MC cell surface FcεRI receptors, or when immune complexes (IgG-ICs) bind to FcγRs, MCs can be activated.
In some cases, such as in mouse BMCMS, the collaboration between FcεRI and inhibitory FcγRIIb can downregulate MC activation. Under antibody/antigen-mediated stimulation, MCs can synthesize and secrete a range of factors (inflammatory factors: TNF-α, IFN-γ, IL-1, 4, 5, 6, 9, 11, 13; regulatory cytokines: IL-10, TGF-β, IL-2, growth factors: IL-3, 6, 9, SCF, GM-CSF; mitogens: FGF-2, VEGF; chemokines: CCL1, 2, 3, 4, 7, 8, 9, 17, 20, 22, CXCL2, 8; granule-associated cytokines: TNF, NGF, VEGF, TGF-β, PDGF, SCF, FGF2).
In turn, these factors can affect other immune and non-immune (structural) cells, leading to various types of allergic reactions, potentially autoimmune diseases like certain forms of arthritis, and host defenses against venoms or parasites. These immune and structural cells comprise functionally distinct subtypes (e.g., T cells, DCs, macrophages, fibroblasts, neurons), and the specific MC products’ effects on these cells can vary significantly depending on the target cell subtype. MC-derived products may also promote tissue repair and remodeling by influencing structural cells and modulating various aspects of the inflammatory/immune response.
Antibody/Antigen-mediated stimulation can also induce MCs to secrete pre-formed mediators such as histamine, serotonin (mainly in rodents), proteoglycans and proteases, as well as certain cytokines and growth factors that may be granule-related, and many lipid mediators, including cysteinyl leukotrienes and certain prostaglandins.
IL-33 is produced by endothelial/epithelial cells at the site of tissue damage, which can stimulate MCs to secrete various factors (IL-4, 5, 6, 13, TNF, CCL1, 2, 3, 17, 22, IL-10, GM-CSF), with different potential effects on other immune and non-immune cells, possibly contributing to the pathogenesis of allergies and host defense.
Pathogen products, such as lipopolysaccharides and peptidoglycans, poly(I:C), and certain viruses can directly activate MCs via TLR (Toll-like receptors), leading to the secretion of various factors (IL-1, 4, 5, 6, 12, 13, TNF, VEGF, GM-CSF, IL-10, CCL2, 4, 8, 20, CXCL2, 8, 10); this may aid in host defense and/or disease (for example, there is a good clinical correlation between certain viral infections and asthma exacerbation).
In Th2-like immune responses, IL-4 or IL-9 from T cells or immature cells in the MC lineage can activate MCs to promote their development and proliferation.
These factors determine the intensity and duration of biological effects.

References
-
Amy Wilcock, Mast cell disorders: From infancy to maturity, Allergy. 2019;74:53–63.
-
Kaori Mukai, Mast cells as sources of cytokines, chemokines, and growth factors, Immunological Reviews. 2018;282:121–150.
-
Michael Stassen, Mast cells within cellular networks, J Allergy Clin Immunol 2019
Source: Chatting Immunology 2019-12-14
